Wellcare Medicare Appeal Form
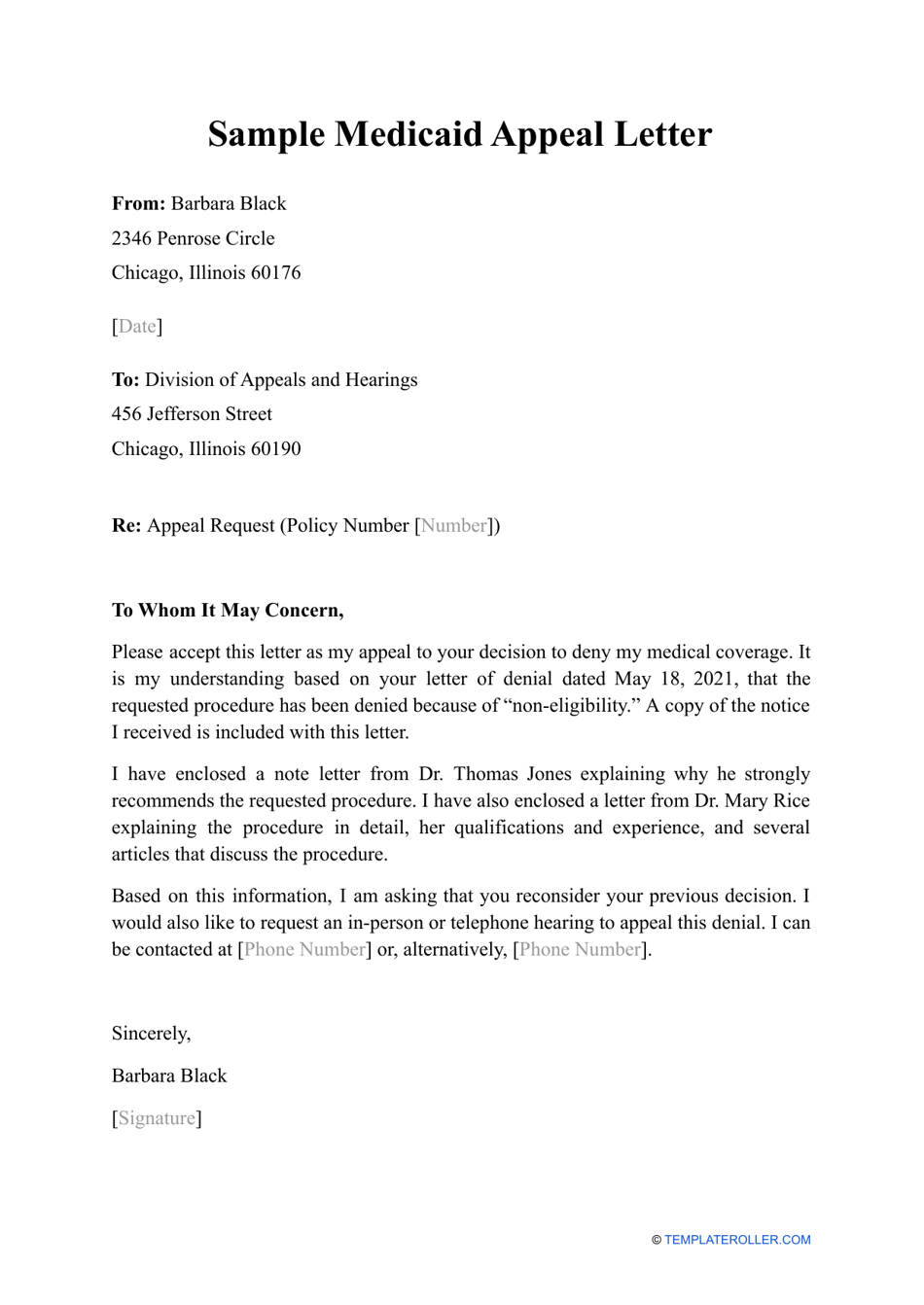
Wellcare Medicare Appeal Form - In the portal, there’s a convenient and easy way to chat with an agent. This form is to be used when you want to reconsider a claim for medical necessity, prior authorization, authorization denial, or benefits. You may file an expedited (fast) appeal by calling member services. Wellcare by allwell medicare requires a copy of the completed and signed appointment of representative form to process. You may fax your standard or. Complete our online request for redetermination of medicare drug denial (part d appeal) form. Visit our provider portal provider.wellcare.com to submit your request electronically. Fill out and submit this form to request prior authorization (pa) for your medicare prescriptions. The provider portal is the fastest way to submit appeals and check status. Complete our online request for redetermination of medicare prescription drug denial (appeal).
This form is to be used when you want to reconsider a claim for medical necessity, prior authorization, authorization denial, or benefits. Fill out and submit this form to. You may file an expedited (fast) appeal by calling member services. In the portal, there’s a convenient and easy way to chat with an agent. Complete our online request for redetermination of medicare prescription drug denial (appeal). Fill out and submit this form to request prior authorization (pa) for your medicare prescriptions. Wellcare by allwell medicare requires a copy of the completed and signed appointment of representative form to process. Complete our online request for redetermination of medicare drug denial (part d appeal) form. The provider portal is the fastest way to submit appeals and check status. Send this form with all pertinent medical documentation to.
Wellcare by allwell medicare requires a copy of the completed and signed appointment of representative form to process. How to file an appeal: In the portal, there’s a convenient and easy way to chat with an agent. Complete our online request for redetermination of medicare drug denial (part d appeal) form. This form is to be used when you want to reconsider a claim for medical necessity, prior authorization, authorization denial, or benefits. The provider portal is the fastest way to submit appeals and check status. Visit our provider portal provider.wellcare.com to submit your request electronically. You may file an expedited (fast) appeal by calling member services. Send this form with all pertinent medical documentation to. Fill out and submit this form to.
Wellcare Tier Exception Form 2023 Printable Forms Free Online
Visit our provider portal provider.wellcare.com to submit your request electronically. Complete our online request for redetermination of medicare prescription drug denial (appeal). In the portal, there’s a convenient and easy way to chat with an agent. The provider portal is the fastest way to submit appeals and check status. How to file an appeal:
Top United Healthcare Appeal Form Templates Free To Download In PDF
Complete our online request for redetermination of medicare prescription drug denial (appeal). How to file an appeal: You may file an expedited (fast) appeal by calling member services. Visit our provider portal provider.wellcare.com to submit your request electronically. Fill out and submit this form to.
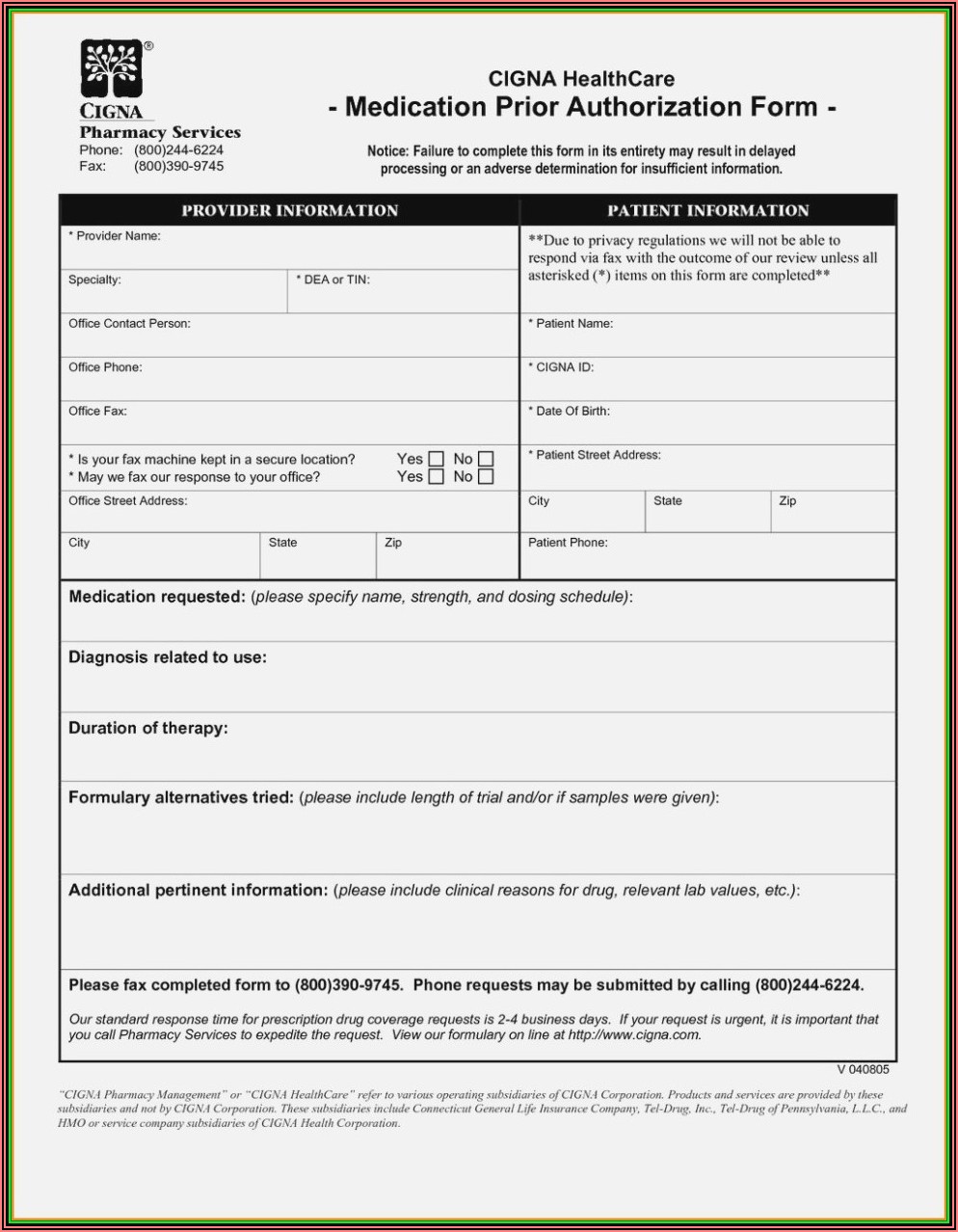
Wellcare Health Plans Medicare Prior Authorization Form
In the portal, there’s a convenient and easy way to chat with an agent. The provider portal is the fastest way to submit appeals and check status. You may file an expedited (fast) appeal by calling member services. Complete our online request for redetermination of medicare prescription drug denial (appeal). Wellcare by allwell medicare requires a copy of the completed.
Wellcare Health Plans Medicare Part D Coverage Determination Request
In the portal, there’s a convenient and easy way to chat with an agent. Complete our online request for redetermination of medicare drug denial (part d appeal) form. Wellcare by allwell medicare requires a copy of the completed and signed appointment of representative form to process. Visit our provider portal provider.wellcare.com to submit your request electronically. You may file an.
Wellcare Medicare Part D Tier Exception Form Form Resume Examples
How to file an appeal: Send this form with all pertinent medical documentation to. Fill out and submit this form to request prior authorization (pa) for your medicare prescriptions. Fill out and submit this form to. You may fax your standard or.
Free WellCare Prior (Rx) Authorization Form PDF eForms
This form is to be used when you want to reconsider a claim for medical necessity, prior authorization, authorization denial, or benefits. Fill out and submit this form to. Send this form with all pertinent medical documentation to. Complete our online request for redetermination of medicare prescription drug denial (appeal). Fill out and submit this form to request prior authorization.
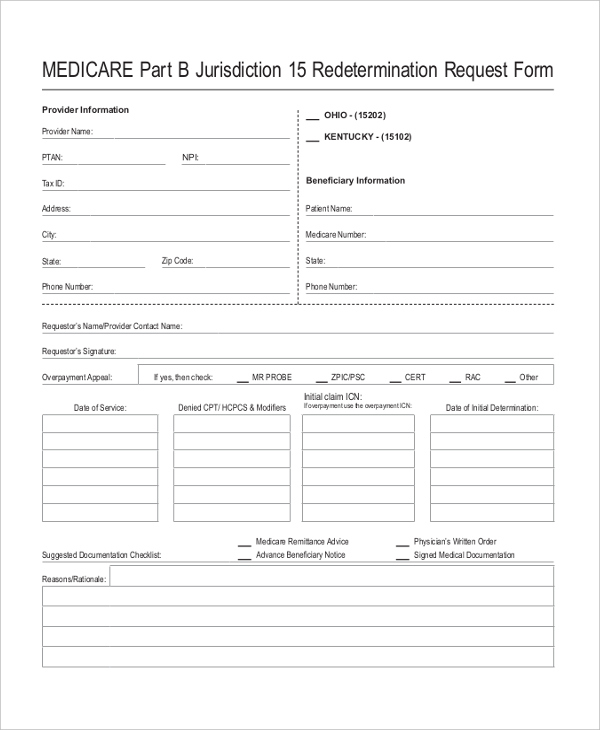
Medicare Appeal Form Cms20027 Medicare (United States) Medicaid
You may fax your standard or. Fill out and submit this form to. The provider portal is the fastest way to submit appeals and check status. Complete our online request for redetermination of medicare drug denial (part d appeal) form. Complete our online request for redetermination of medicare prescription drug denial (appeal).
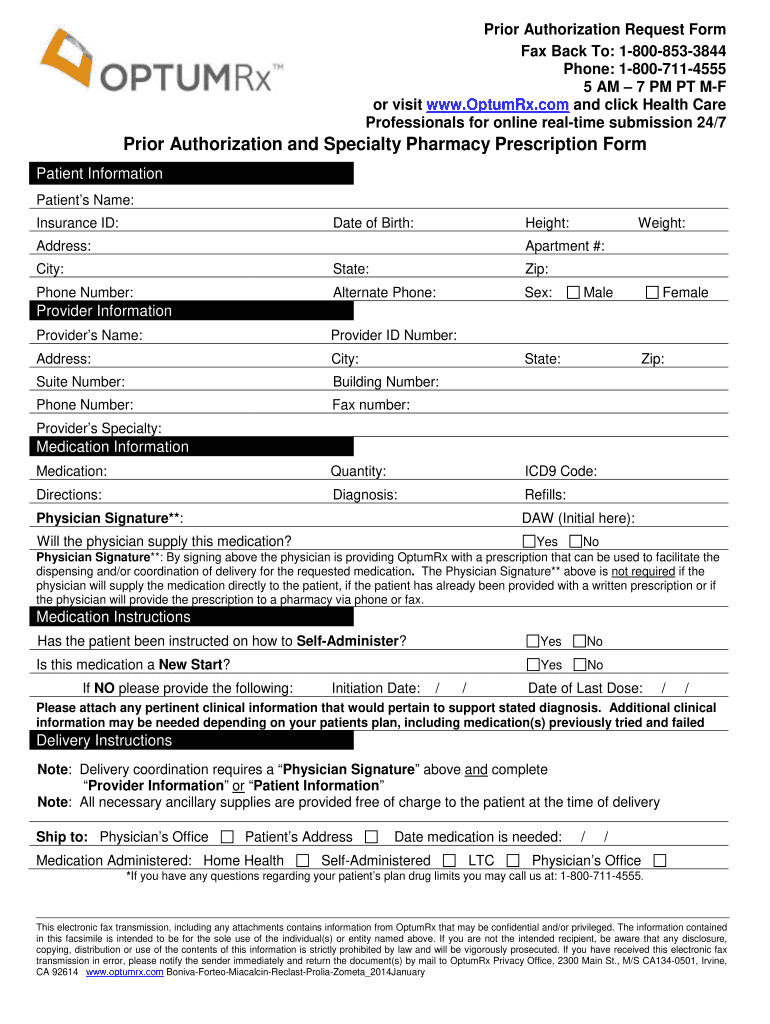
Optum Rx Appeal Form Complete with ease airSlate SignNow
Fill out and submit this form to request prior authorization (pa) for your medicare prescriptions. In the portal, there’s a convenient and easy way to chat with an agent. Complete our online request for redetermination of medicare drug denial (part d appeal) form. How to file an appeal: You may fax your standard or.
FREE 10+ Sample Medicare Forms in PDF MS Word
Complete our online request for redetermination of medicare prescription drug denial (appeal). Fill out and submit this form to. The provider portal is the fastest way to submit appeals and check status. In the portal, there’s a convenient and easy way to chat with an agent. How to file an appeal:
Medication Letter Of Medical Necessity Template
You may fax your standard or. Send this form with all pertinent medical documentation to. This form is to be used when you want to reconsider a claim for medical necessity, prior authorization, authorization denial, or benefits. Complete our online request for redetermination of medicare prescription drug denial (appeal). You may file an expedited (fast) appeal by calling member services.
Fill Out And Submit This Form To.
Visit our provider portal provider.wellcare.com to submit your request electronically. You may fax your standard or. Complete our online request for redetermination of medicare prescription drug denial (appeal). You may file an expedited (fast) appeal by calling member services.
How To File An Appeal:
Send this form with all pertinent medical documentation to. Wellcare by allwell medicare requires a copy of the completed and signed appointment of representative form to process. In the portal, there’s a convenient and easy way to chat with an agent. Fill out and submit this form to request prior authorization (pa) for your medicare prescriptions.
The Provider Portal Is The Fastest Way To Submit Appeals And Check Status.
Complete our online request for redetermination of medicare drug denial (part d appeal) form. This form is to be used when you want to reconsider a claim for medical necessity, prior authorization, authorization denial, or benefits.